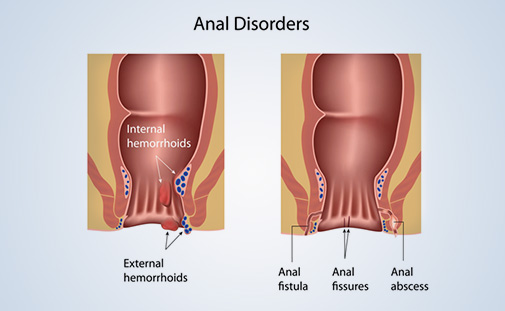
Anal polyps are small growths on the inner lining of the rectum. They can be classified as benign or malignant (cancerous). The risk of cancer is strongly associated with the type and size of the polyp you have.
- Safety First COVID-19
-
Treatments
-
Orthopaedic Surgery
- Arthroscopic knee surgery
- Arthroscopic meniscectomy
- Anterior cruciate ligament (ACL) surgery
- Bunion surgery
- Carpal tunnel release
- Chondropathy surgery
- Cubital tunnel release
- Dupuytren’s contracture surgery
- Ganglion Removal
- Hammertoe surgery
- Hip replacement surgery
- Laser Disc Decompression (PLDD)
- Patellar dislocation
- Shoulder surgery
- Total knee replacement
- General Surgery
- Hand surgery
- Gynecological surgery
- ENT Surgery
- Ophthalmic Surgery
- Diagnostics
- Urological surgery
- Proctology
-
Orthopaedic Surgery
- Prices
- Our hospital
- Our Team
- Travel Guide
- Blog
- Contact